Medical Billing Outsourcing Market By Component (In-House, Outsourced), By Service Type (Back-End, Middle-End, Front-End), By End-User (Hospitals, Physicians, Other), By Region And Companies - Industry Segment Outlook, Market Assessment, Competition Scenario, Trends, And Forecast 2023-2032
-
16350
-
May 2023
-
174
-
-
This report was compiled by Correspondence Linkedin | Detailed Market research Methodology Our methodology involves a mix of primary research, including interviews with leading mental health experts, and secondary research from reputable medical journals and databases. View Detailed Methodology Page
-
Quick Navigation
Report Overview
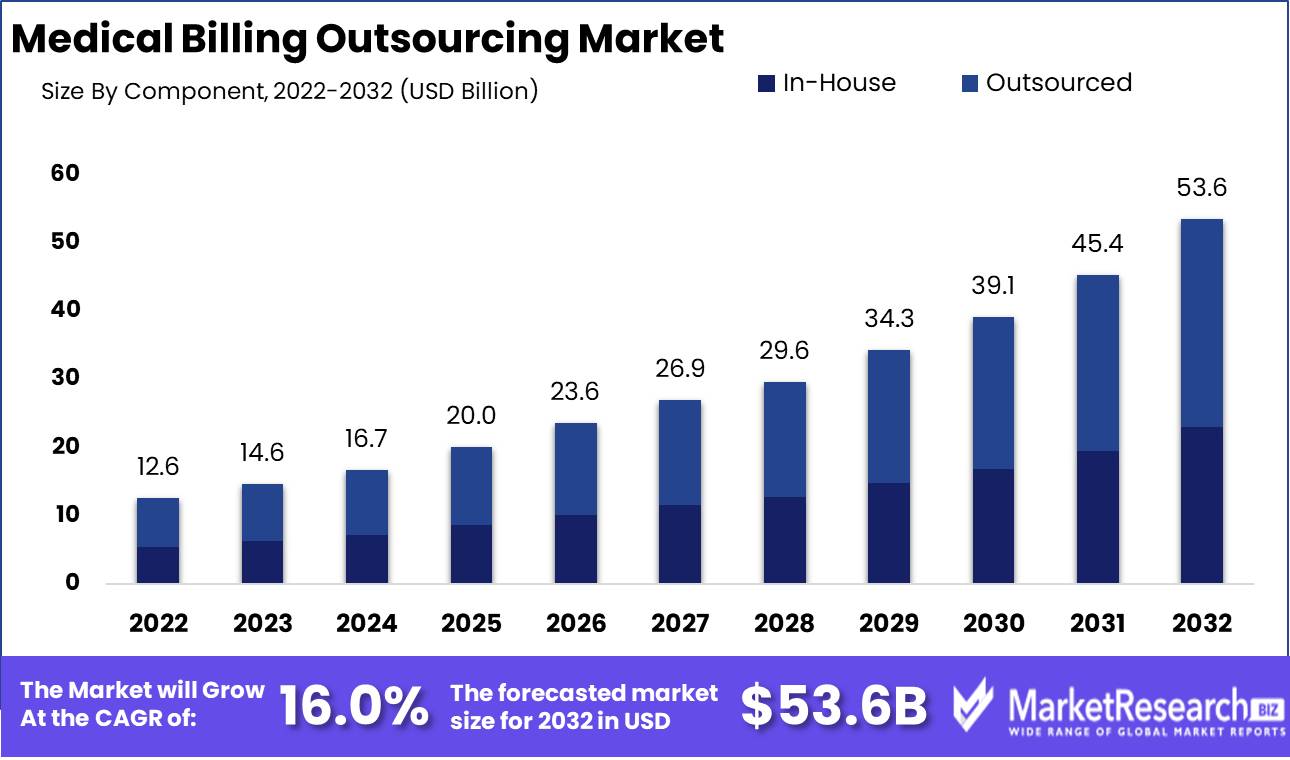
Medical Billing Outsourcing Market size is expected to be worth around USD 53.6 Bn by 2032 from USD 12.6 Bn in 2022, growing at a CAGR of 16.0% during the forecast period from 2023 to 2032.
Outsourcing has gained significant prevalence across various industries and sectors, including the healthcare industry. In recent years, there has been a notable increase in the adoption of medical billing outsourcing within the healthcare industry. This trend can be attributed to the desire of healthcare providers to optimize their operational processes and improve their financial management capabilities. The medical billing outsourcing market consists of healthcare providers who opt to delegate their billing and revenue management procedures to specialized third-party service providers.
The importance of outsourcing medical billing cannot be overstated. Healthcare providers, including hospitals, clinics, and individual practitioners, often encounter challenges when it comes to effectively managing their billing procedures. The field of medical billing encompasses a range of duties, such as the submission of claims, the posting of payments, the management of denials, and the billing of patients. The aforementioned duties require proficiency and expertise in coding, insurance regulations, and billing software. By delegating these responsibilities to proficient experts, healthcare providers can guarantee prompt and precise reimbursement.
There exist a multitude of advantages that are closely linked to the practice of outsourcing medical billing. It provides healthcare providers with access to specialized knowledge. Medical billing companies typically hire professionals who possess expertise in coding, billing regulations, and industry best practices. Healthcare providers can effectively utilize their expertise to ensure the submission of precise claims and mitigate the potential for noncompliance with billing regulations. The outsourcing of medical billing has the potential to effectively mitigate the administrative burdens experienced by healthcare providers.
Significant advancements have been observed within the medical billing outsourcing industry. The incorporation of artificial intelligence (AI) and machine learning (ML) technologies into medical billing procedures represents a notable advancement in this field. Artificial intelligence (AI) and machine learning (ML) algorithms have the capability to automate monotonous billing tasks, such as claim validation, coding, and submission. This automation leads to enhanced productivity and accuracy. Furthermore, the utilization of these technologies allows healthcare providers to enhance their revenue cycle and identify areas for improvement by analyzing historical billing data to identify patterns and trends.
In recent years, there has been a significant influx of investment in the market for outsourcing medical billing services. The potential of outsourcing to improve the financial administration of healthcare providers has been acknowledged by numerous healthcare technology companies and venture capital firms. These investments have contributed to the growth of the market, leading to the emergence of new competitors and the expansion of existing ones. AI in Revenue Cycle Management is revolutionizing the Medical Billing Outsourcing Market, streamlining processes for faster reimbursements and reduced errors.
Driving factors
Increasing Medical Billing Complexity
As the healthcare business evolves, medical billing systems have become more complicated. Regulations, medical technology, and insurance policies all contribute to this complexity. Medical billing is more than just claims and payments. From proper coding to insurance and regulatory compliance, it includes several complex stages. These processes involve painstaking attention to detail, considerable knowledge of medical codes and vocabulary, and the ability to navigate rigorous payment guidelines. This intricacy might overwhelm healthcare providers, who already have to provide quality care.
Healthcare Industry Growth
Due to rising population, aging demographics, and medical technology, the healthcare industry has grown significantly. Demand for healthcare services rises as the sector grows, increasing patient contacts and medical procedures. Healthcare providers must manage more patient records, insurance claims, and billing processes due to this expansion. It can be challenging to manage these enormous numbers efficiently and accurately. Outsourcing medical billing services can help.
Changing Insurance and Reimbursement
Insurance and reimbursement are crucial to medical billing. These policies vary frequently as governments and insurance firms respond to new rules and market conditions. Healthcare providers must monitor and comprehend complex rules to keep up with these developments. The medical billing processes are complicated by changing reimbursement and insurance policies. To get paid quickly, claims must be coded, documented, and submitted correctly. Claim denials, delayed payments, and legal issues might occur from not following the newest policies.
Increased EHR Adoption
In recent years, the healthcare business has adopted EHR. EHRs increase patient care coordination, healthcare provider information exchange, and data security. However, integrating EHR systems into medical billing processes presents obstacles. Data transfer, correct documentation, and code alignment are needed to integrate EHR systems with medical billing. EHR systems and their functions must be understood for these activities. Non-expert healthcare professionals may struggle to use EHR platforms for billing.
Cost Containment and Efficiency Needed
Cost control and operational efficiency are essential for healthcare firms in a competitive market. Healthcare providers' revenue cycles might suffer from inefficient, error-prone, or resource-intensive medical billing processes. Outsourcing medical billing services solves these issues. Healthcare providers can enhance revenue cycle management, minimize administrative costs, and improve operational efficiency by working with billing businesses. These outsourcing agencies optimize billing procedures, reduce errors, and increase revenues using their expertise, industry experience, and technology infrastructure.
Restraining Factors
In-house billing departments
The medical billing outsourcing market may also be hampered by in-house billing departments. Many healthcare providers have internal billing departments that may fear job loss from outsourcing. An internal billing team may discourage outsourcing due to the company's training and development. Outsourcing billing may worry in-house billing departments about layoffs or diminished roles. If outsourcing occurs, workers may feel intimidated. Thus, they may oppose outsourcing medical billing.
Compliance and Regulations
Potential regulatory and compliance requirements affect the medical billing outsourcing market. Healthcare rules defend patient rights, assure fair billing, and uphold ethical standards. Whether they outsource or manage billing in-house, healthcare providers must comply with these rules. Medical billing outsourcing requires a rigorous regulatory audit of potential vendor partners. Healthcare providers should verify their outsourcing partner understands these standards and can demonstrate compliance.
Knowledge Transfer and Communication Issues
Efficient information transfer and good communication are critical for medical billing. Healthcare practitioners outsourcing their knowledge and skills may face hurdles. Miscommunication and process misalignment can disrupt billing and postpone payments. Knowledge transfer requires documentation, clear communication, and best practices. To guarantee a smooth transition, extensive training, collaboration, and support are needed.
Patient-Provider Relationships
Patient-provider connections are a major medical billing outsourcing market restraint. Patient data, insurance claims, and financial transactions make medical billing complicated. Any disruptions or inaccuracies in the billing process can damage patient trust. Outsourcing medical billing may distance patients from their providers. Lack of direct involvement can reduce accountability and openness, affecting patient-provider interactions.
Medical Billing Outsourcing Excellence
Healthcare providers can handle medical billing outsourcing market challenges to gain its benefits. Successful outsourcing requires thorough due diligence, partner selection, and patient and internal stakeholder communication. Outsourcing medical billing can save money, improve accuracy, and access advanced technologies. In today's fast-paced, complex healthcare environment, providers should carefully consider outsourcing their medical billing processes.
Component Analysis
Outsourced Segment dominates medical billing outsourcing market. The field of medical billing outsourcing has experienced significant growth in recent years, with the outsourced segment dominating the market. This segment involves outsourcing medical billing and coding tasks to specialized firms, allowing healthcare providers to focus on their core responsibilities.
Consumer trends and behavior also play a crucial role in the dominance of the outsourced segment. Patients are increasingly becoming more informed and involved in their healthcare decisions, demanding greater transparency and accuracy in medical billing processes. By outsourcing these tasks to specialized firms, healthcare providers can ensure that their patients are receiving accurate bills and have a clear understanding of the services provided.
Service Type Analysis
Front-End Segment dominates medical billing outsourcing market. In the medical billing outsourcing market, the front-end segment holds a dominant position. The front-end segment involves tasks such as patient registration, insurance verification, and appointment scheduling. These tasks play a crucial role in the smooth functioning of healthcare facilities and providers.
Consumer trends and behavior also contribute to the dominance of the front-end segment. Patients now expect a seamless and convenient experience when interacting with healthcare providers. By outsourcing front-end tasks, healthcare providers can ensure that patients have a smooth registration process and convenient appointment scheduling, meeting their expectations and improving patient satisfaction.
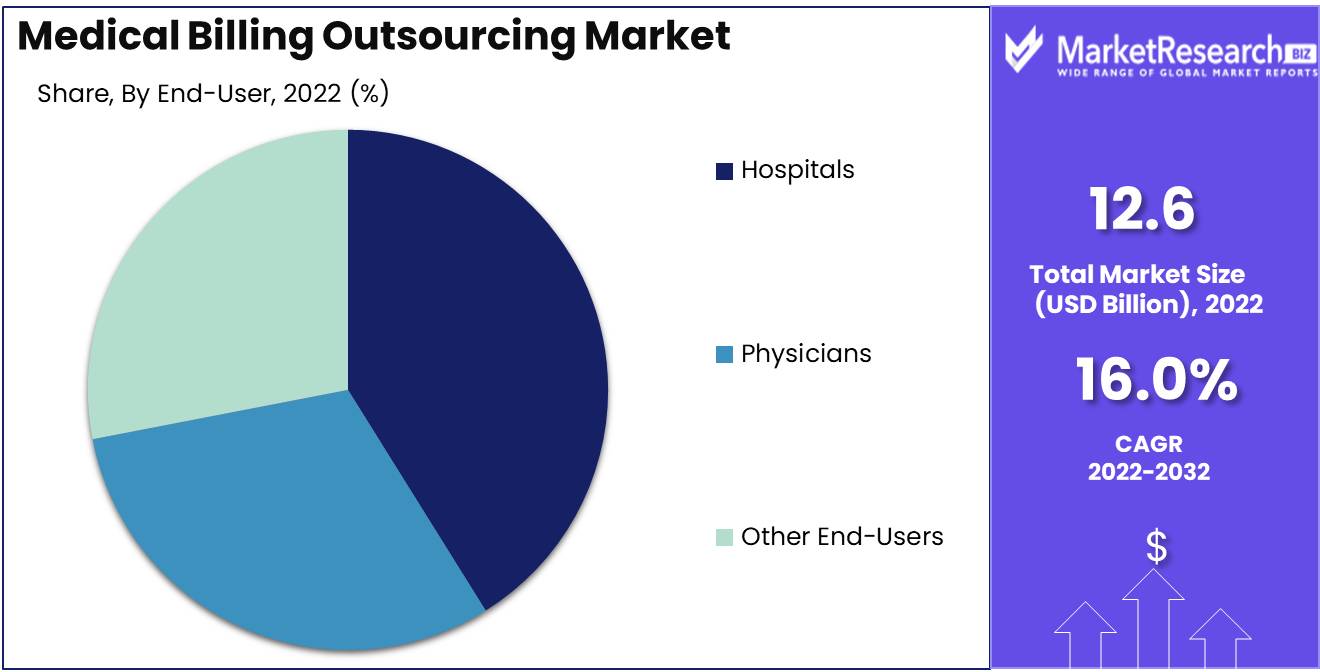
End-User Analysis
Hospitals Segment dominates medical billing outsourcing market. The hospitals segment holds a dominant position in the medical billing outsourcing market. Hospitals have unique billing requirements due to the breadth and complexity of their services. Outsourcing medical billing tasks to specialized firms allows hospitals to focus on patient care while ensuring accurate and efficient billing processes.
Consumer trends and behavior also influence the dominance of the hospitals segment. Patients often seek specialized care and rely on hospitals for complex treatments and procedures. By outsourcing medical billing tasks, hospitals can ensure accurate billing and provide patients with a transparent understanding of the services rendered. This enhances patient satisfaction and trust in the healthcare system.
Key Market Segments
By Component
- In-House
- Outsourced
By Service Type
- Back-End
- Middle-End
- Front-End
By End-User
- Hospitals
- Physicians
- Other End-Users
Growth Opportunity
Medical Billing Outsourcing Security
In the digital world, organizations across industries prioritize security. The medical billing outsourcing market follows suit. Companies offering medical billing outsourcing services with enhanced security are seeing more opportunities as healthcare providers realize the importance of patient data privacy and HIPAA compliance. Healthcare firms face serious financial and reputational risks from data breaches and cyberattacks. Medical billing outsourcing organizations can protect patient information with innovative technologies and strong security measures.
Medical Billing Outsourcing AI
The medical billing outsourcing market is growing rapidly due to AI technologies. AI-based solutions boost productivity, accuracy, and cost-effectiveness, helping medical billing outsourcing organizations streamline operations and revenue cycle management. AI is used for medical billing outsourcing. AI-powered software may extract patient data from medical records, bills, and other documents, eliminating data entry and errors. Automation speeds up billing, improves accuracy, and decreases administrative strain on healthcare practitioners.
Value-Based Care Expansion
Medical billing outsourcing organizations can assist value-based care by expanding their service offerings. Value-based care emphasizes quality over quantity to improve patient outcomes and lower costs. Medical billing outsourcing companies can help healthcare providers satisfy performance-based metrics and negotiate reimbursement models based on patient outcomes by aligning their services with value-based care concepts. They can help manage and report clinical quality measurements, capture patient data for outcome evaluations, and optimize value-based care reimbursement schemes.
Latest Trends
Leveraging Specialized Outsourcing
Outsourcing medical coding and claims processing services has proven to be an incredibly effective strategic move for healthcare organizations of all sizes. By partnering with specialized outsourcing providers, these organizations can tap into a vast pool of highly skilled professionals who possess a deep understanding of medical coding guidelines, industry regulations, and insurance policies.
Denial Management and Revenue Recovery
The demand for denial management and revenue recovery services has skyrocketed, prompting healthcare providers to seek expert assistance. Properly managing claim denials and swiftly recovering revenue can significantly impact the financial health of healthcare organizations. Outsourced denial management services offer a comprehensive approach to identifying denial hotspots, analyzing root causes, and implementing preventive measures. Through robust data analysis, outsourcing providers can uncover patterns, identify recurring issues, and implement targeted strategies to reduce denials and improve revenue recovery, ultimately enhancing the bottom line.
Transforming Claims Accuracy
Predictive analytics, one of the most significant technological advancements in the healthcare industry, is radically transforming claims accuracy and reimbursement optimization. Leveraging advanced algorithms and machine learning techniques, predictive analytics enables healthcare providers to proactively identify potential errors, ensure claims accuracy, and optimize reimbursement rates. By leveraging historical data and identifying patterns, predictive analytics can streamline claims processing, reduce coding errors, and minimize claim rejections.
Specialized Support
The rise of value-based reimbursement models and bundled payment systems has necessitated the need for specialized support services. These alternative payment models focus on quality outcomes rather than the traditional fee-for-service approach. To succeed in this paradigm shift, healthcare providers are turning to outsourcing partners that can provide comprehensive support in navigating the complexities of value-based reimbursement. From data analysis to performance reporting, outsourcing providers offer tailored solutions to ensure compliance, accurate coding, and maximize reimbursements in line with value-based models.
Unprecedented Growth
The medical billing outsourcing market is witnessing unprecedented growth, driven by the increasing demand for operational efficiency, cost reduction, and accurate reimbursements. To stay ahead in this rapidly evolving landscape, healthcare organizations must embrace outsourcing as a strategic imperative. Outsourcing medical coding and claims processing services provides a multitude of benefits, including but not limited to access to specialized expertise, enhanced revenue recovery, reduced denials, improved claims accuracy, and proactive error prevention.
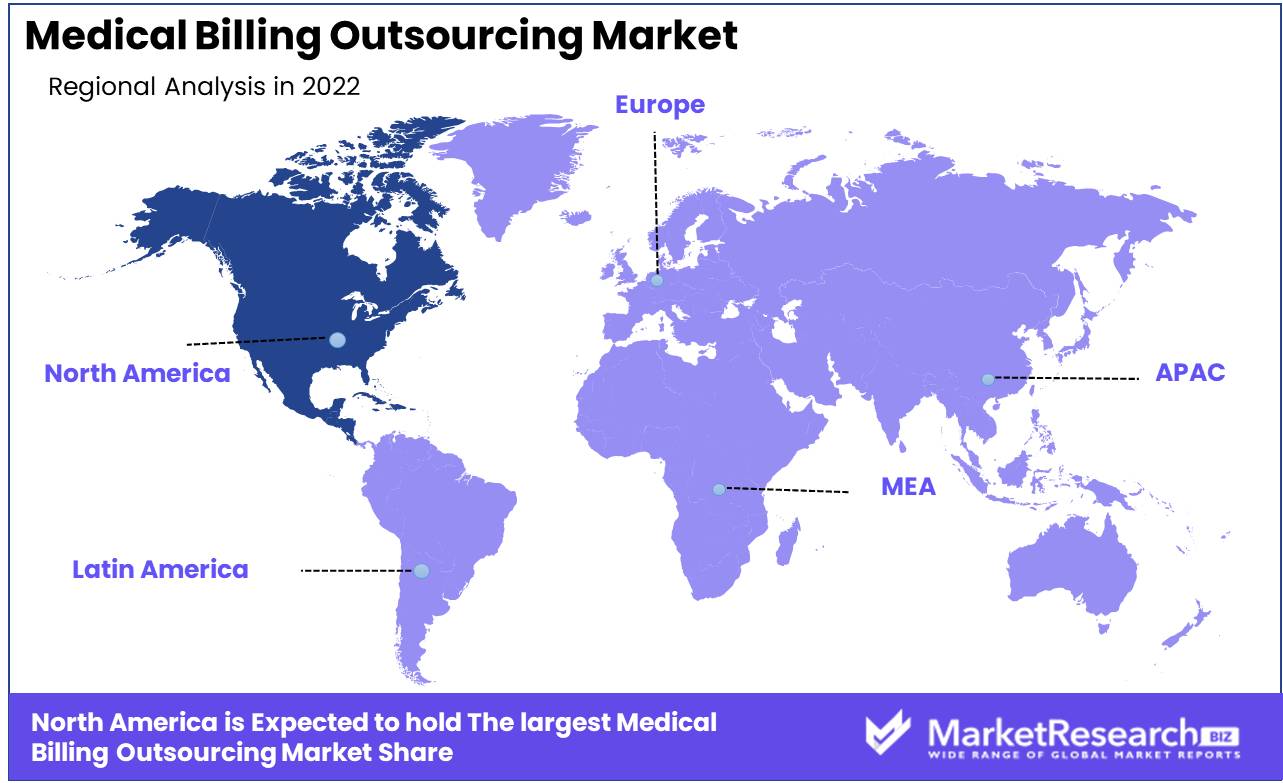
Regional Analysis
North America dominates the market for medical billing outsourcing. In today's ever-changing healthcare environment, outsourcing medical billing has become a necessity for healthcare providers pursuing efficiency, cost-effectiveness, and enhanced revenue cycle management. With its robust infrastructure, sophisticated technology, and skilled labor force, North America has become the leading player in the medical billing outsourcing market.
Medical billing is a highly specialized field that requires in-depth knowledge of coding systems, insurance protocols, and complex reimbursement processes. By outsourcing this vital task to specialized service providers, healthcare providers can concentrate on providing quality patient care while leaving the complexities of billing and revenue management to the experts.
The dominance of North America in the medical billing outsourcing market can be attributed to a number of significant factors. Initially, the region is home to a mature healthcare industry that seeks innovative ways to streamline operations. As a result, the demand for outsourcing services has skyrocketed, leading to the establishment of a large number of specialized companies that provide comprehensive medical billing services.
The region's technologically sophisticated infrastructure is crucial to its dominance. With cutting-edge billing software, electronic health record systems, and seamless connectivity, North American service providers can provide accurate, timely, and efficient billing services to all sizes of healthcare providers. This technology-driven strategy not only ensures compliance with stringent industry standards, but also enables seamless integration with diverse healthcare systems, thereby augmenting data privacy, security, and overall efficiency.
Key Regions and Countries
North America
- US
- Canada
- Mexico
Western Europe
- Germany
- France
- The UK
- Spain
- Italy
- Portugal
- Ireland
- Austria
- Switzerland
- Benelux
- Nordic
- Rest of Western Europe
Eastern Europe
- Russia
- Poland
- The Czech Republic
- Greece
- Rest of Eastern Europe
APAC
- China
- Japan
- South Korea
- India
- Australia & New Zealand
- Indonesia
- Malaysia
- Philippines
- Singapore
- Thailand
- Vietnam
- Rest of APAC
Latin America
- Brazil
- Colombia
- Chile
- Argentina
- Costa Rica
- Rest of Latin America
Middle East & Africa
- Algeria
- Egypt
- Israel
- Kuwait
- Nigeria
- Saudi Arabia
- South Africa
- Turkey
- United Arab Emirates
- Rest of MEA
Key Players Analysis
Healthcare providers can focus on their primary strengths while outsourcing medical billing to specialist organizations. R1RCM Inc., Cerner Corporation, Allscripts Healthcare LLC, Experian Information Solutions Inc., eClinicalWorks, and General Electric dominate the medical billing outsourcing market, and we will examine them in this post.
US-based R1RCM Inc. dominates the medical billing outsourcing market. R1RCM has streamlined medical billing operations, reduced costs, and improved revenue cycle management for healthcare providers with its highly qualified employees and cutting-edge technology.
Cerner Corporation is another major competitor in the medical billing outsourcing market that provides comprehensive healthcare technology solutions. Cerner Corporation integrates medical billing services to improve efficiency and patient outcomes.
Allscripts Healthcare LLC is known for its unique medical billing outsourcing services. Allscripts Healthcare LLC helps healthcare providers improve billing, revenue, and profitability by using innovative technology and industry knowledge.
Data-driven analytics and credit services are Experian's specialty. Experian optimizes revenue cycle performance for healthcare providers in the medical billing outsourcing market via data analysis. Experian helps healthcare firms maximize financial performance by discovering revenue leakage, minimizing claim denials, and improving reimbursement rates.
eClinicalWorks provides medical billing outsourcing and other healthcare administration services. eClinicalWorks delivers a single platform for patient care and revenue management by effortlessly integrating medical billing into their EHR system. Their revolutionary strategy ensures medical billing accuracy, efficiency, and compliance.
Industrial innovator General Electric has made important contributions to the medical billing outsourcing market. General Electric uses process optimization and advanced analytics to improve billing accuracy, claim denials, and revenue cycle management for healthcare providers.
Top Key Players in Medical Billing Outsourcing Market
- R1RCM Inc. (US)
- Cerner Corporation (US)
- Allscripts Healthcare LLC (US)
- Experian Information Solutions Inc .(US)
- eClinicalWorks (US)
- General Electric (US)
- Genpact (US)
- Kareo,Inc. (US)
- McKesson Corporation (US)
- Quest Diagnostics Incorporated (US)
- The SSI Group LLC (US)
- Athenahealth Inc (US)
- 5 Star Billing Service Inc (US)
- Experian Information Solutions Inc. (US)
Recent Development
- In 2023, Patient Financial Services (PFS) will be acquired by healthcare giant Accretive Health. PFS is a top medical billing outsourcing company with extensive experience. This acquisition strengthens Accretive Health's revenue cycle management and market position in a competitive market.
- In 2022, CHG Healthcare acquired MedData, another medical billing outsourcing company, last year. This strategic investment will allow CHG Healthcare to leverage MedData's significant experience and synergies to expand revenue cycle management. Industry leaders constantly change and expand their services.
- In 2021, Conifer Health Solutions acquired 3M Health Information Systems to boost expansion and service. This innovative partnership combines Conifer Health Solutions' expertise with 3M's medical billing outsourcing. This acquisition will enable Conifer Health Solutions to meet market demands and provide comprehensive revenue cycle management solutions.
- In 2020, RCM Solutions acquired MedAvante, a top medical billing outsourcing company, last year. RCM Solutions aligns with MedAvante's billing expertise by expanding its capabilities. RCM Solutions becomes a market leader in revenue cycle management with the purchase.
Report Scope:
Report Features Description Market Value (2022) USD 12.6 Bn Forecast Revenue (2032) USD 53.6 Bn CAGR (2023-2032) 16% Base Year for Estimation 2022 Historic Period 2016-2022 Forecast Period 2023-2032 Report Coverage Revenue Forecast, Market Dynamics, COVID-19 Impact, Competitive Landscape, Recent Developments Segments Covered By Component (In-House, Outsourced)
By Service Type (Back-End, Middle-End, Front-End)
By End-User (Hospitals, Physicians, Other End-UsersRegional Analysis North America – The US, Canada, & Mexico; Western Europe – Germany, France, The UK, Spain, Italy, Portugal, Ireland, Austria, Switzerland, Benelux, Nordic, & Rest of Western Europe; Eastern Europe – Russia, Poland, The Czech Republic, Greece, & Rest of Eastern Europe; APAC – China, Japan, South Korea, India, Australia & New Zealand, Indonesia, Malaysia, Philippines, Singapore, Thailand, Vietnam, & Rest of APAC; Latin America – Brazil, Colombia, Chile, Argentina, Costa Rica, & Rest of Latin America; Middle East & Africa – Algeria, Egypt, Israel, Kuwait, Nigeria, Saudi Arabia, South Africa, Turkey, United Arab Emirates, & Rest of MEA Competitive Landscape R1RCM Inc. (US), Cerner Corporation (US), Allscripts Healthcare LLC (US), Experian Information Solutions Inc .(US), eClinicalWorks (US), General Electric (US), Genpact (US), Kareo,Inc. (US), McKesson Corporation (US), Quest Diagnostics Incorporated (US), The SSI Group LLC (US), Athenahealth Inc (US), 5 Star Billing Service Inc (US), Experian Information Solutions Inc. (US) Customization Scope Customization for segments, region/country-level will be provided. Moreover, additional customization can be done based on the requirements. Purchase Options We have three licenses to opt for: Single User License, Multi-User License (Up to 5 Users), Corporate Use License (Unlimited User and Printable PDF) -
-
- R1RCM Inc. (US)
- Cerner Corporation (US)
- Allscripts Healthcare LLC (US)
- Experian Information Solutions Inc .(US)
- eClinicalWorks (US)
- General Electric (US)
- Genpact (US)
- Kareo,Inc. (US)
- McKesson Corporation (US)
- Quest Diagnostics Incorporated (US)
- The SSI Group LLC (US)
- Athenahealth Inc (US)
- 5 Star Billing Service Inc (US)
- Experian Information Solutions Inc. (US)